Tuberculosis (TB) is relatively rare in the U.S., but when a case is identified, it typically triggers a response from public health officials to reduce the risk of transmission. JoAnne Flynn, Ph.D., a professor of microbiology and molecular genetics at the University of Pittsburgh School of Medicine and Pitt’s Center for Vaccine Research, answers common questions about the infectious disease.
Tuberculosis (TB) is relatively rare in the U.S., but when a case is identified, it typically triggers a response from public health officials to reduce the risk of transmission. JoAnne Flynn, Ph.D., a professor of microbiology and molecular genetics at the University of Pittsburgh School of Medicine and Pitt’s Center for Vaccine Research, answers common questions about the infectious disease.
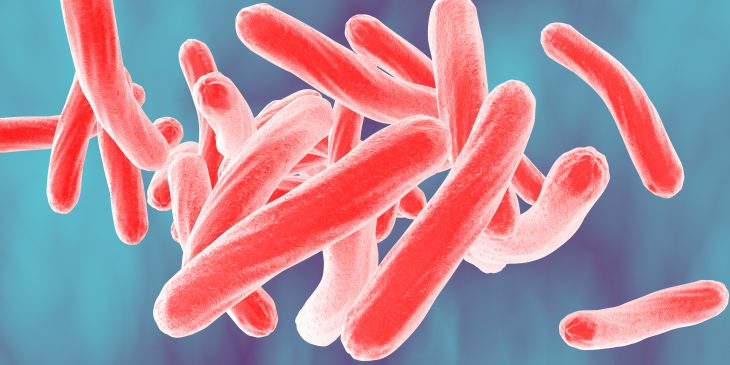
What is tuberculosis and why is it a serious health threat?
Tuberculosis is a lung disease caused by the bacterium Mycobacterium tuberculosis. An active infection is characterized by a cough that lasts several weeks, weight loss and difficulty breathing. If left untreated, it can cause lung damage. The majority of people who become infected do not develop active TB and remain asymptomatic. This is referred to as “latent TB,” and it’s considered to be non-contagious.
TB diagnosis involves a skin test or a blood test. If positive, these tests only indicate that someone is infected, not whether he or she has active TB. Further testing to confirm active infection includes chest x-ray or CT, as well as sputum culture.
How is it transmitted?
The infection is transmitted from a person with active TB by coughing, talking, sneezing or even singing. The bacteria are then breathed in by another person, which results in infection 30% of the time. Transmission is more common when people are in close contact, especially for extended periods of time.
What is the treatment?
Treatment of active TB involves four different and specialized antibiotics—the regimen is four drugs for two months, followed by two of those drugs for another four months.
Treatment for latent TB varies. It involves taking one or two drugs for three to nine months. Such treatment reduces the chance for re-emergence of the infection in the person with latent TB.
Is there a vaccine for TB?
We do not vaccinate against TB in the United States because our rates of TB are low.
The vaccine is a live, but crippled, version of the bacterium and is given to infants in most countries around the world. It is effective against the worst manifestations of childhood tuberculosis, but has variable efficacy against active tuberculosis. It is not clear why the vaccine works better in some populations than others, nor why the vaccine is not more effective.
How could the vaccine be improved?
It seems that sustained immune responses against the bacterium may be necessary for long-term protection. There are preclinical studies that support new ways to vaccinate that may be more effective, but these await clinical trials to prove efficacy.
What are you discovering in the lab that could be used to combat tuberculosis infections?
Our studies have led to a better understanding of the disease, as well as new drugs and vaccines against the infection.
What are the biggest challenges right now for TB treatment and prevention?
Better and more rapid diagnostics are essential for quickly finding people with active TB. Because the symptoms can evolve slowly, people do not get diagnosed in a timely fashion, increasing the risk that they can spread the infection to others before they start treatment.
There has also been an emergence of drug-resistant strains of the bacteria, which are not cured by the standard treatment. Drug resistance testing takes additional time. There is hope though – for the first time in years, new medications that are more effective against drug-resistant strains have come to market.
HIV is a major risk factor for developing tuberculosis. Understanding how HIV and TB interact is important in reducing TB numbers worldwide.
Overall, a much more effective vaccine is essential for TB eradication.