A protein called IL-17 can train cells in the lymph nodes to help mice better fight future infections, according to a recent study published in Science Immunology.
This finding, if it applies to humans, may explain why certain childhood vaccinations provide broad protection from diseases beyond the one a child is immunized against.
“A great example of this unexpected benefit is the BCG vaccine. In Europe, this vaccine has been shown to reduce the overall childhood mortality rate by providing protection from not only tuberculosis — the disease that BCG vaccination targets — but from other diseases as well. This may be, in part, due to the concept of innate immune training,” said Dr. Mandy McGeachy, senior author of the study and associate professor of medicine and immunology at the University of Pittsburgh.
Human immune systems have two branches: innate and adaptive. Innate immunity is our first line of defense against pathogens and also gives directions to our adaptive immune system. During infection, T and B cells of the adaptive immune system form memory cells, so that they can respond more quickly if faced with the same pathogen down the road.
Although the innate immune system lacks this memory, recent research indicates that this system can be “trained” during infection to respond more quickly and efficiently to future, unrelated infections.
In the new study, McGeachy and her team investigated whether innate immune training in mice could protect against common gut infections. In humans, gut infections caused by pathogens such as E. coli are the second leading cause of infection-related deaths in children under age 5 worldwide, according to the World Health Organization.
Immune cells “train” mouse lymph node cells to better fight future infections
To simulate innate immune training, the researchers treated mice with DSS, a chemical often used to induce gut inflammation in mice. They found that these animals were better protected from subsequent infection with Citrobacter rodentium — a bacterium that causes gut symptoms — compared to mice that had not received immune training.
Importantly, “trained” mice also had better antibody responses and cleared the infection with less gut damage.
“Our findings that causing mild gut inflammation is actually protective for the future may seem a little counterintuitive,” said McGeachy. “But if you think about babies and children who initially get many infections, they eventually reach a point where they don’t get so sick with each new infection. It seems as if one infection helps tune the immune system to respond to new infections with less damaging inflammation, even if it’s not the same pathogen each time.”
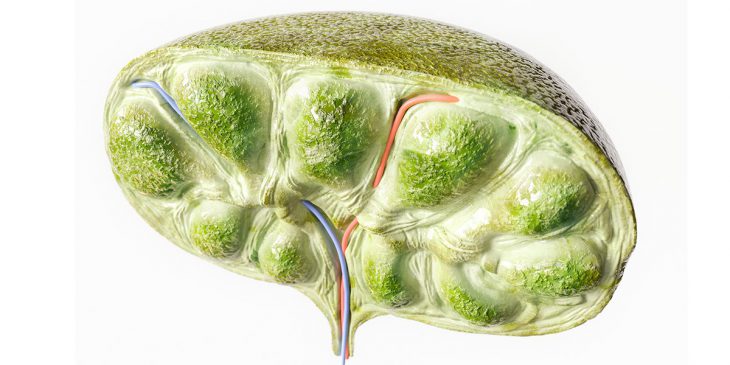
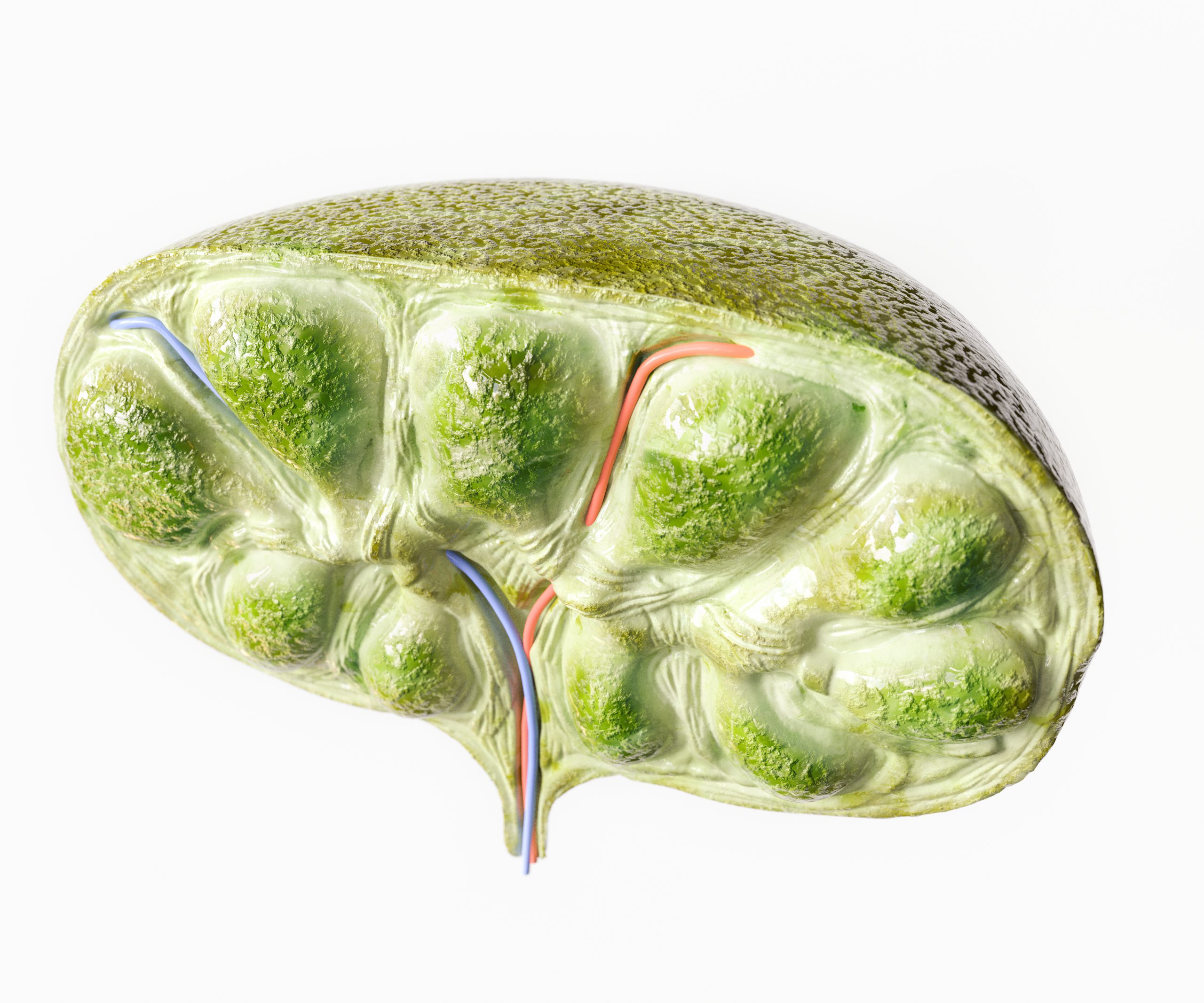
The researchers found that mice with prior gut inflammation had more fibroblastic reticular cells, or FRCs, a type of cell that gives structure to our lima bean-shaped lymph nodes. These FRCs had DNA changes that suggested they had been trained to respond to C. rodentium, despite never having been exposed to the pathogen.
In addition to providing a place for immune cells to meet up, FRCs also “talk” with immune cells, exchanging proteins to instruct each cell to perform specific functions. The researchers suspected that in response to DSS-induced inflammation, immune cells train FRCs via an inflammatory protein called IL-17.
To test this hypothesis, McGeachy and her team genetically modified mice so that their FRCs lacked IL-17 receptors, meaning they could not “hear” the IL-17 signal. When they provided immune training with DSS followed by immune challenge with C. rodentium, the mice did not exhibit an increase in the number of FRCs as in the unmodified mice. Mice that were “deaf” to IL-17 also had worse antibody response and more gut inflammation, indicating that IL-17 was responsible for training the FRCs.
McGeachy was surprised that IL-17 was behind this beneficial immune response.
“We usually associate IL-17 with diseases where inflammation is in overdrive,” said McGeachy. “But it also has a role in protecting us during infection, and we are starting to understand more about its beneficial effects. IL-17 is not such a bad guy after all.”
In the future, McGeachy hopes that the concept of innate immune training could improve therapeutic and vaccine design.
“If we can design new vaccines that incorporate ways to train our lymph node cells, such as FRCs, we may be able to favor immune responses that not only help us clear infection but also help us avoid excessive inflammation.”
Haylee Baxendell is a Ph.D. candidate in the University of Pittsburgh School of Medicine’s Program in Microbiology and Immunology. She is participating in the UPMC Science Writing Mentorship Program.